The liver is a vital organ responsible for several essential functions, including the metabolism of xenobiotics – substances foreign to the body, such as drugs – aiming for their elimination. Consequently, the liver is frequently exposed to a wide range of xenobiotics, including pharmaceuticals and their metabolites. Unfortunately, this also makes the liver susceptible to drug-induced liver injury (DILI), a leading cause of acute liver failure associated with a high fatality rate. DILI is one of the most common reasons for drug withdrawals from the market, and over a third of newly approved therapeutics are labelled with hepatotoxicity warnings. Identifying potential DILI hazards and liabilities early during lead optimization can help de-risk the chance of major setbacks at the later stages of drug development programs.
One of the most well-known examples of DILI is paracetamol (acetaminophen), which can lead to intrinsic DILI, when taken in excessively high doses. In such cases, the amount of toxic metabolites produced exceed the reduction capacity of glutathione, which would normally detoxify these metabolites for renal excretion. As a result, the toxic metabolites interact with cellular macromolecules and accumulation of these actions leads to liver necrosis. This type of DILI is predictable, occurs shortly after the drug exposure and is dose responsive. Compounds causing intrinsic DILI are often lipophilic and expose the hepatocytes to oxidative stress by forming reactive oxygen species, disrupting the mitochondrial function and altering bile acid flow e.g. by inhibiting BSEP (bile salt export pump). Also, disturbances in lipid homeostasis such as increased lipid accumulation is typically one of the early signs of hepatotoxicity.
In contrast, idiosyncratic DILI is unpredictable and multifactorial, with factors such as age, gender, genetics, environmental influences, or immune responses playing a role. The timing of onset can vary significantly, making idiosyncratic DILI more challenging to anticipate and mitigate. For idiosyncratic DILI, it is challenging to find a suitable preclinical testing battery.
The mechanisms leading to DILI are complex, and currently, its occurrence cannot be tested with a single in vitro assay which would translate well to an in vivo situation. Similarly, in vivo models are often not fully predictive of human outcomes. To follow the 3R principles (Replacement, Reduction, Refinement), animal testing should be kept to a minimum. Over the past years, various in vitro tools have been developed further, applying cellular systems and more human-like conditions to the assay. New approach methods (NAMs) for the testing of chemicals and drugs, are of great interest, often combining various in vitro data with sophisticated safety modeling in silico tools (e.g. PBPK, read-across), together providing an alternative yet also human-relevant testing approach. In addition, with the aid of adverse outcome pathway (AOP) network information, it is possible to predict biological outcomes of drugs by extrapolating from available data, without use of animals. An AOP describes a series of events at different levels of the organism (cell, tissue, organ), that lead to an adverse effect, followed by an insult. The ongoing research in this area is very active, resulting in novel AOPs and allowing probably even more toxicity testing according to the 3R principle, in the (near) future.
Typically, the methods applied for initial screening for DILI are rather simple 2D cultures with easy handling and scalability to HTS, used to investigate cellular viability in addition to the known mechanisms behind idiosyncratic DILI. The applied methods, even in early screening, should employ human hepatocytes, which provide the most comprehensive metabolic system and also contain relevant membrane transporters in comparison to many other systems in use. The measured endpoints include assessing cytotoxicity and cell viability (e.g. ATP, MTT or LDH, dead-cell protease assays), since the ultimate consequence of hepatic insult is hepatocyte necrosis and liver failure. Induction of oxidative stress and reactive oxygen species (ROS) is one of the key mechanisms and is often measured in the cells. Altered mitochondrial function is also one of the typical hepatotoxicity mechanisms, and assessing it is usually a crucial part of DILI screening (e.g. Glu/Gal assay, Seahorse). Furthermore, formation of reactive metabolites and inhibition of membrane transporters are typically investigated when DILI liabilities are considered. All these techniques have their own limitations, and hence, multiple tests should be conducted for effective screening of potential DILI liabilities.
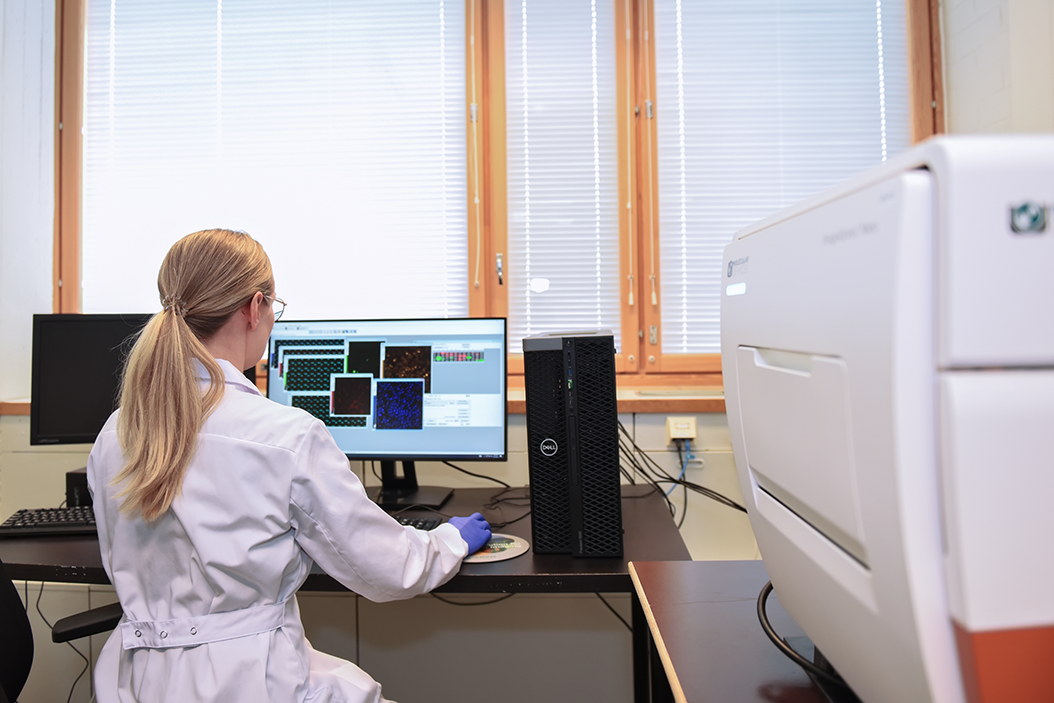
In more advanced approaches, imaging technologies are employed to measure multiple endpoints from the same incubations, effectively providing a more comprehensive understanding of cellular responses and mechanisms causing hepatotoxicity. Automation of these processes enhances data robustness, improves assay throughput, and accelerates turnaround times—critical factors for the success of drug development projects. This integration of imaging and automation not only streamlines workflows but also enables higher data quality and faster decision-making. Going further, more complex cellular systems such as organoids and other microphysiological systems (MPS) can be used as part of DILI assessment for testing drug candidates, providing even more physiological relevance to the assay, thus aiming to capture the more rare, idiosyncratic DILI events at the later stages of drug development.
If you are wondering whether your project has a DILI liability, feel free to reach out to our experts to discuss the topic further!